2021 KAISER FAMILY FOUNDATION —
The COVID-19 pandemic has taken a heavy toll on people in nursing homes, with those in long-term care facilities accounting for a disproportionate share of all deaths attributable to COVID-19 to date. However, less attention has been paid to nonelderly people with disabilities who use long-term services and supports (LTSS) but live outside of nursing homes. This population includes people with a range of disabilities, such as people with autism or Down’s syndrome who live in group homes, people with physical disabilities who receive personal care services at home, and people who are receiving behavioral health treatment in residential facilities.
Some nonelderly people with disabilities receive LTSS in a variety of community-based settings such as group homes, adult day health programs, and/or their own homes. Other nonelderly people with disabilities receive LTSS in institutional settings such as intermediate care facilities for people with intellectual or developmental disabilities (ICF/IDDs) or behavioral health treatment centers for people with mental illness or substance use disorder. Many nonelderly people with disabilities, both in the community and in institutions, rely on Medicaid as the primary payer for the LTSS on which they depend for meeting daily self-care needs.
Nonelderly people with disabilities and the direct care workers who provide their LTSS have similar risk factors for serious illness or death from COVID-19 compared to their counterparts in nursing homes, due to the close contact required to provide assistance with daily personal care tasks, such as eating, dressing, and bathing; the congregate nature of many of these settings; and the highly transmissible nature of the coronavirus. Seniors in nursing homes are explicitly included in the top priority group in all states’ COVID-19 vaccine distribution plans, but nonelderly people with disabilities who use LTSS may be not prioritized.
This issue brief presents current state-level data about COVID-19 cases and deaths in settings that primarily serve nonelderly people with disabilities and summarizes available research on this population’s elevated risk of severe illness and death; explains how nonelderly people with disabilities and their LTSS providers are reflected in state vaccine prioritization plans; and discusses key issues related to vaccine access for these populations.
What is known about COVID-19 among people with disabilities?
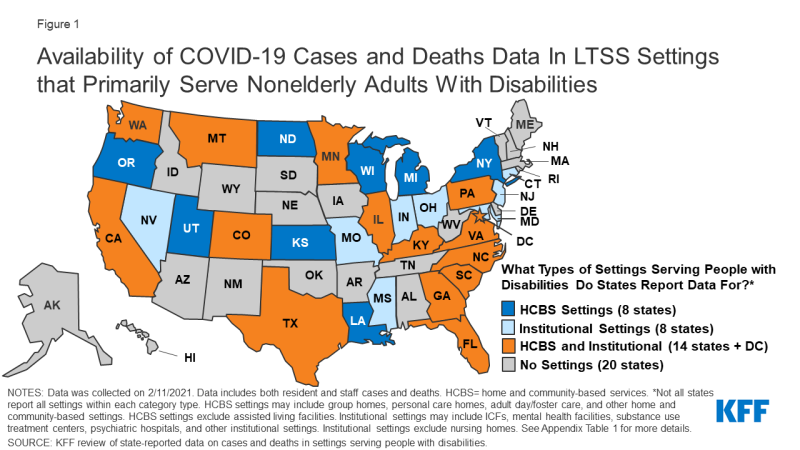
As of February 11, 2021, 31 states report at least some data on COVID-19 cases and deaths in LTSS settings that primarily serve nonelderly people with disabilities (Figure 1 and Appendix Table 1).
These settings include both home and community-based settings such as group homes, personal care homes, adult day programs, and other community-based settings; and institutional settings such as intermediate care facilities and psychiatric institutions.
Not all states report all types of settings within each category. These data exclude settings that primarily serve elderly adults, such as nursing facilities and assisted living facilities (ALFs), to best reflect cases and deaths solely among nonelderly adults with disabilities. For state-level data broken out by resident/staff cases/deaths, details on the types of facilities included in each state’s count, dates of data, links to the state reports, and additional notes, see Appendix Table 1.
Figure 1: Availability of COVID-19 Cases and Deaths Data In LTSS Settings that Primarily Serve Nonelderly Adults With Disabilities
‘Apples to apples’ comparisons difficult
The wide variety in state reporting makes it difficult to compare between states or have a complete understanding of how people with disabilities have been impacted by the pandemic.
Among states reporting data, there were 111,000 cases and over 6,500 deaths across these settings as of February 11, 2021 (Figure 1).
Of the 31 states reporting data, 8 states report data only for institutional settings, 8 states report data only for home and community-based settings, and 15 states report data for both settings.
Thirty-one states report cases and 25 states report deaths. States also vary in whether they report only data on residents and staff separately or combined (Appendix Table 1). State reporting also varies in other ways, such as inclusion of only active cases (e.g., MA, UT), inclusion of data within broader long-term care reporting (e.g., ID, MD, MS, OK, GA, KY, LA, NC, ND), and level of detail in facility-level information. Additionally, states use different definitions or categorizations for the same types of facilities, making cross-state comparison challenging.
Data from a limited number of states suggest that LTSS residents in institutions other than nursing and assisted living facilities, as well as those in some community-based settings, face an elevated risk of COVID-19 infection (Table 1). Overall, limited data on the number of people in HCBS and institutional settings other than nursing and assisted living facilities makes calculating case or death rates difficult. However, eight states (CT, IL, NJ, OR, PA, WA, WI, TX) provide resident census data to calculate the shares of residents that have been impacted in certain settings.
Among the states that provide census data on institutional settings, cumulative data show that between 19% (Connecticut’s mental health facilities) and 50% (Pennsylvania’s state centers for individuals with intellectual disabilities) of residents were infected. These rates are on par with the share of residents infected in nursing homes, which, using 2019 resident census data and resident case counts as of the end of January 2021, is about 50%. These rates are also higher than population level rates, which show more than 8% of the US population infected as of mid-February 2021.
For states that provide census data on home or community-based settings, between 2% (Oregon’s Adults with Intellectual or Developmental Disabilities Foster Care HCBS waiver) and 19% (Illinois’ Community Integrated Living Arrangements group homes) of residents were infected. Given the limited sample size and wide state variation, this data should be interpreted with caution. However, this data supports other research suggesting that congregate settings, particularly larger facilities, are at high risk of having an outbreak.
| Table 1: Share of Residents Who Were Infected with Coronavirus in Selected State Settings | |||
| Residents Coronavirus Cases | Resident Census | Share of Residents Infected With Coronavirus | |
| Home and Community-Based Settings | |||
| Illinois Community Integrated Living Arrangements | 1,859 | 9,992 | 19% |
| Oregon ODDS Services – Adult DD Foster Care | 66 | 2,928 | 2% |
| Oregon ODDS Services – Adult DD Group Homes | 155 | 3,022 | 5% |
| Washington DDA Community Residential Service Providers | 668 | 4,500 | 15% |
| Wisconsin HCBS Waiver: IRIS | 1,381 | 22,332 | 6% |
| Wisconsin HCBS Waiver: Managed Long-Term Care | 8,155 | 55,009 | 15% |
| Institutional Settings | |||
| Connecticut DMHAS Facilities | 142 | 760 | 19% |
| New Jersey State Psychiatric Facilities | 332 | 1,151 | 29% |
| Pennsylvania State Centers | 321 | 640 | 50% |
| Pennsylvania State Hospitals | 560 | 1,348 | 42% |
| Texas State Supported Living Centers | 1,302 | 2,777 | 47% |
| Texas State Hospitals | 715 | 1,678 | 43% |
|
NOTES: Data are “as of” various dates; data was collected on 2/11/2021. These settings were selected based on states that specified a resident census count upon which certain case counts were based. Resident census counts in each setting reflect multiple facilities/residences. See Appendix Table 1 for links to state reports.
SOURCE: KFF analysis of state-reported data on cases and deaths in settings serving people with disabilities.
|
|||
COVID risk in other setting similar to that in nursing homes
Other research shows that nonelderly people with disabilities who receive LTSS in settings other than nursing homes face similar COVID-19 risk factors compared to people in nursing homes.
Like those in nursing homes, people with disabilities rely on the close physical proximity of caregivers for communication and daily needs, which limits their ability to adopt preventive measures such as social distancing. An October 2020 study found that people with I/DD living in group homes in New York are at greater risk of contracting and dying from COVID-19 compared to the general population.
Another study from July 2020 found greater risk for contracting COVID-19 among people with I/DD, and a greater case fatality rate for nonelderly adults with I/DD, compared to those without I/DD. A November 2020 analysis of private insurance claims found that people with “developmental disorders” (such as speech/language, scholastic skills, and central auditory processing disorders) had the highest odds of dying from COVID-19 and those with intellectual disabilities (such as Down’s syndrome) had the third highest risk of death from COVID-19.
Continue reading at KFF.org