From NextAvenue.org —
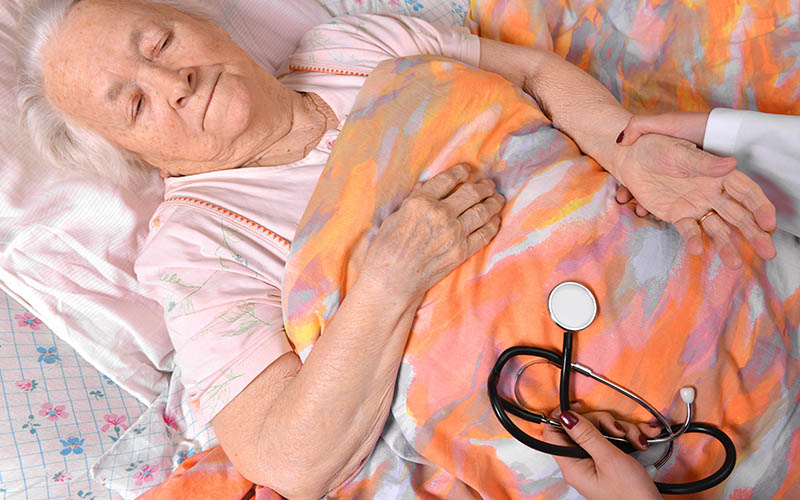
Who are the essential workers paid to care for America’s aged in their homes and in residential and nursing care facilities?
The past year-and-a-half has put an unprecedented spotlight on the care received by America’s aging population. There’s been a renewed focus on the essential workers who do the hard, uncelebrated labor of tending to their daily, even hourly, personal, physical, emotional and social needs.
The past year-and-a-half has put an unprecedented spotlight on the care received by America’s aging population. There’s been a renewed focus on the essential workers who do the hard, uncelebrated labor of tending to their daily, even hourly, personal, physical, emotional and social needs.
Compensation for their labor is low and their pay has remained stagnant even as hundreds of thousands of families have come to depend on them and the demand for their work continues to expand.
Federal data released in 2020 said that these paid caregivers earned a median wage of $13 an hour. That number swings higher in large metropolitan areas and lower in less populated regions; the hourly mean wage in San Francisco is $16.57, while caregivers in small Texas communities in the Rio Grande Valley earn $9.54 an hour.
“These wages are not livable or competitive; forty-five percent of these workers live in low-income households,” said Robert Espinoza, vice president of policy for PHI, an organization focused on strengthening the direct care workforce (who is a Next Avenue Influencer in Aging). “Many leave for better paying jobs with more stable schedules in retail or fast food. Direct-care jobs are often misrepresented as low- or no-skilled work, but because of the responsibility they assume and the emotional component they bring, that’s just wrong.”
Maria: Doing Extra on the Job
While the rest of the world is waking up, Maria Marrero is on the job.
A certified home health aide for low-income older clients in New Jersey, her first stop is in the home of a man with dementia. She helps him out of bed, bathes and dresses him and prepares and feeds him breakfast. When his family caregiver relieves her midmorning, Marrero goes up a floor to client No. 2, a patient with Parkinson’s disease, and performs many of the same tasks.
It’s early afternoon when she arrives at the home of a married couple in their eighties. The husband is slowed by congestive heart disease and his frail wife has osteoporosis. Marrero tends to their personal needs, does their laundry, cleans, reminds them to take their medications, cooks and keeps them company.
“Sometimes my people say, ‘Don’t do nothing today, just sit and talk.’ This is how lonely they feel,” said Marrero. “I bring the lady in the wheelchair in the kitchen with me while I make the lunch and do the dishes. She wants the companionship, but I have work to do.”
Marrero began taking care of older people at age 11, helping a neighbor in her native Puerto Rico. Later, after marrying, arriving in New Jersey and giving birth to three daughters, she began working through a home health agency, a job she’s performed for 18 years.
“My husband drives a truck and I could not afford to do this if he didn’t have a good job,” she said. “I love my seniors, but we who do this are invisible, sad to say. I work with all my heart. I do extra. But I get stuck on the same payment for years.”
Unfair Share of the Burden
In 2019, before the coronavirus arrived, the federal government had issued a 10-year projection that anticipated that the demand for direct-care workers would surge, with 1.3 million new jobs added by 2029.
Attracting adequate numbers of workers to take those jobs was already challenging, but the pandemic made efforts to recruit and retain direct care staff far trickier.
“Shortages went through the roof. A lot of nursing homes were already not staffed at levels we think are sufficient to meet the needs of their vulnerable residents, and the pandemic exacerbated that,” said Lori Smetanka, executive director of The National Consumer Voice, which advocates for policy to improve long-term care for patients, their families and the direct-care workforce.
When co-workers called in sick, extra shifts and stress levels rose sharply among direct-care staff. Smetanka believes they’ve continued to shoulder an unfair share of the burden brought on by the virus.
“Their workload increased tremendously. They have concerns about their own well-being and that of their families. They were dealing with inadequate supplies as the virus came through the door. Many of them got sick and some died,” said Smetanka.
She tracks legislation pending in a few states that would require upgraded staffing levels and Congressional action that would dedicate money to staff compensation, actions that could edge working conditions in the right direction.
“When people come to his job, we hear them say it’s their calling. They like the close relationships with residents. We want to encourage that, but we need to improve pay and benefits so these are quality jobs that people want to keep,” Smetanka said.
She predicts a steep climb to fill the gap of unfilled caregiving jobs without significant policy changes.
“We keep asking them to do more and don’t give them the supports they need,” Smetanka sighed. “Unfortunately, there’s not the will to address these issues in a meaningful way.”
Continue reading at NextAvenue.org